Our Research
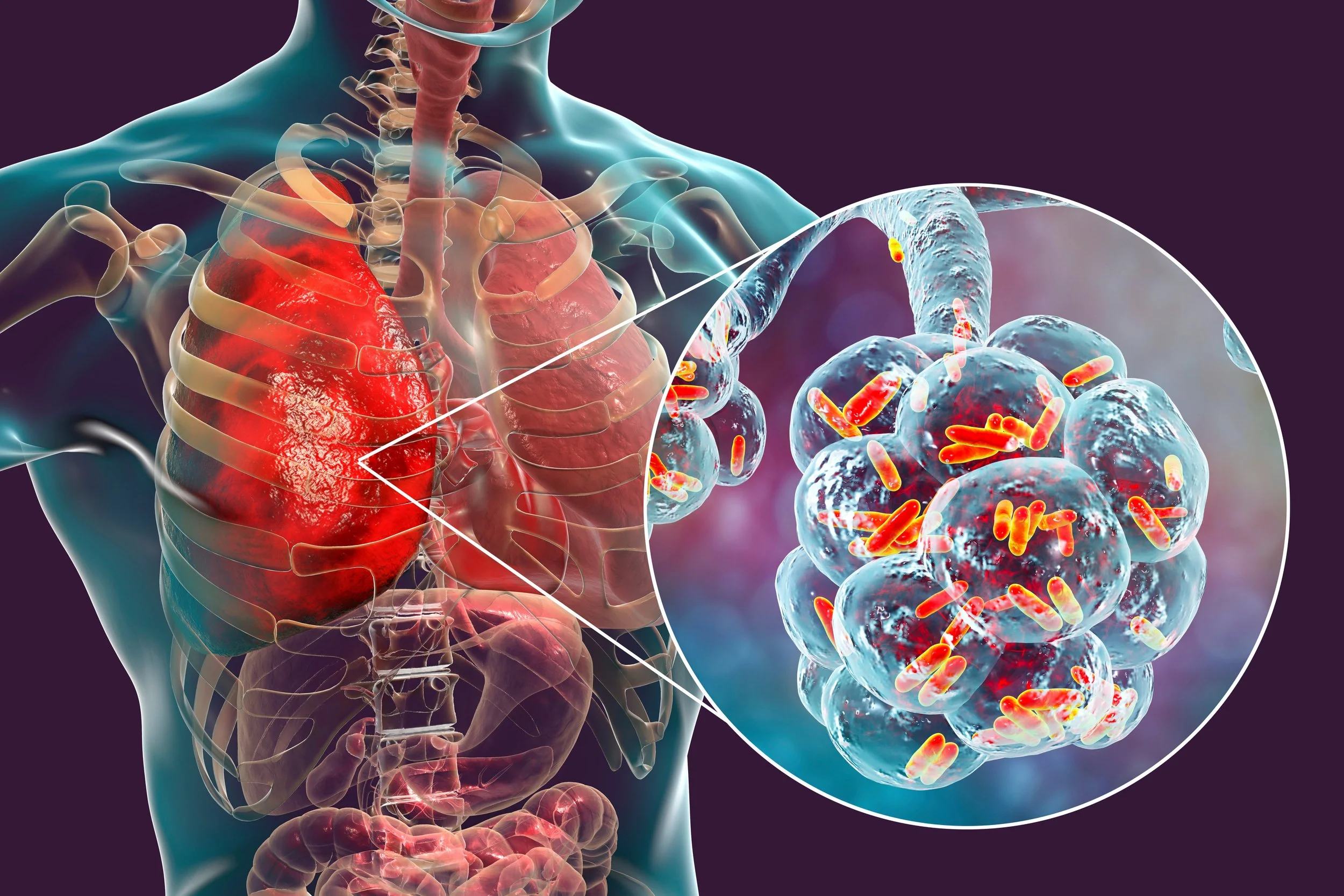
Respiratory diseases are particularly debilitating conditions and are significant drivers of healthcare costs.
Our immune system is set up to combat bacterial infections, however, when lung function is compromised, the interactions between human cells and the bacteria are changed and increase infection severity and duration.
Environmental pollution, including bushfires, or underlying conditions such as asthma, bronchiectasis, Chronic Obstructive Pulmonary Disease or Cystic Fibrosis are causes of diminished lung function.
Our target pathogen, Haemophilus influenzae, is highly prevalent in patients suffering from chronic lung diseases. H. influenzae is host-adapted, which means that it is completely adapted to surviving in the human respiratory tract, its only natural niche.
How do pathogenic bacteria survive during infection?
Haemophilus influenzae and other bacterial pathogens are remarkably resistant to a range of antibacterial chemicals produced by the immune system during infection. We are investigating the molecular mechanisms that enable this resistance, which interestingly includes several evolutionarily ancient enzyme.
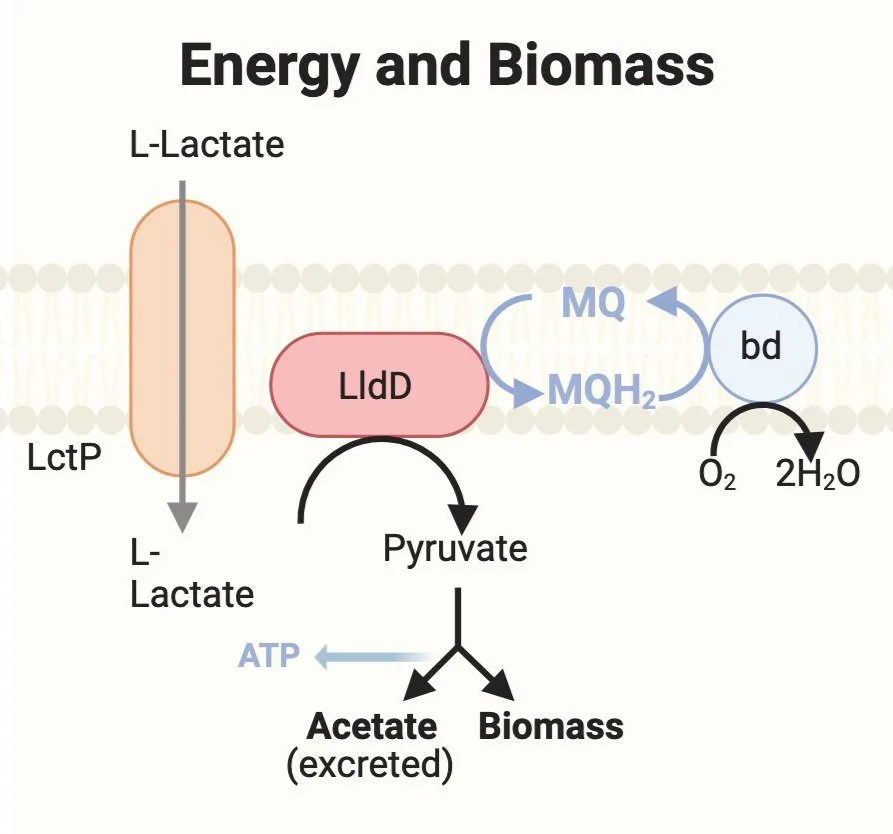
What kinds of nutrients support H. influenzae pathogenesis?
Host-adapted bacteria such as H. influenzae are highly adapted to survival in the human body, and that includes adaptation to using available food sources. If you are interested in which types of nutrient molecules support H. influenzae during contact with host cells, please click below.
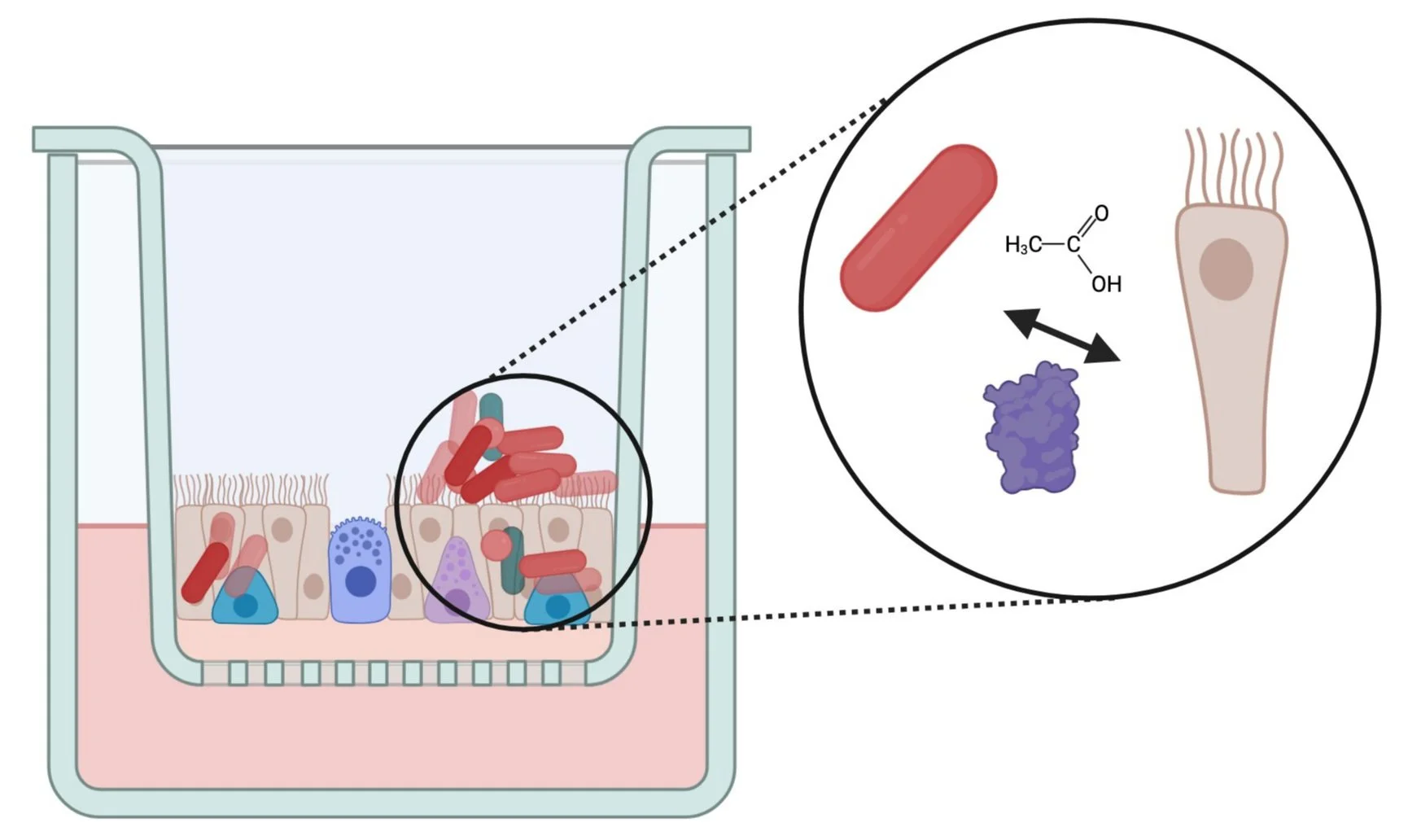
Why are chronic infections with H. influenzae so common?
H. influenzae can colonize the outside of respiratory tract epithelial cells, but also manages to establish itself inside human cells within the first 24h of infection. We have recently shown that H. influenzae colonization leads to a reduced and delayed immune response to infection.
Images created with BioRender